Gene therapy in Duchenne
Gene therapy research represents cutting-edge science, but the treatment approach is not new. Gene therapy research actually dates back to the 1960s. Since then, multiple treatments have been approved for diseases like cancer, hemophilia, spinal muscular atrophy, and others.
Decades of research have focused on how gene therapy might help treat genetic conditions like Duchenne. Let's take a look at what researchers have learned so far.
Jump ahead to: How it's designed to work | Who it may be appropriate for | How it's studied in trials
How gene therapy is designed to work
With Duchenne, the body doesn’t make enough dystrophin, a protein muscles need to work properly. Gene therapy aims to address this by putting a new gene inside muscle cells. The goal for this new gene is to give the cells instructions in hopes of making a working version of the dystrophin protein.
The dystrophin gene, or DMD gene, is the largest in the human body, which can make it difficult to deliver to cells. To get around this challenge, researchers are looking at how to use only the most important parts of the original gene. This allows them to see if the combination they chose for the new gene can help cells produce dystrophin. It would be a different kind of dystrophin than the body makes naturally, but one that's designed to do the same job.
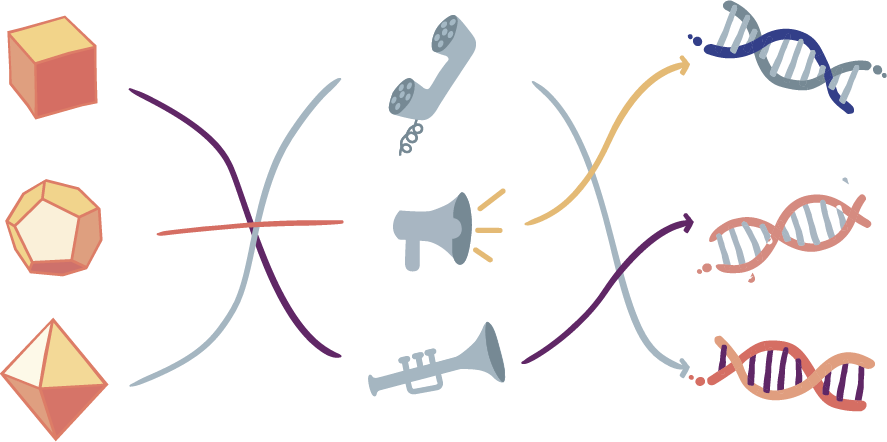
Each gene therapy is made of 3 main parts: A vector, a promoter, and a transgene.
The 3 components are designed to work together to help the body make a different, but working, version of the protein.
Each gene therapy is unique, even when they are designed to treat the same disease. Which vector, promoter, and transgene scientists select can impact how well the gene therapy might work and the side effects a person may have. That's why scientists rigorously test different combinations in a laboratory before selecting the final pieces and beginning clinical trials.
Eligibility, or who gene therapy may be appropriate for
Every gene therapy is different, so each has unique guidelines about who may be eligible for treatment. Many things go into determining eligibility, which a doctor can explain. However, there are 2 important criteria anyone considering Duchenne gene therapy should understand:

Confirming a Duchenne diagnosis
This is accomplished through a genetic test that looks for a change, or mutation, in the dystrophin gene.

Testing for specific antibodies in the blood
This test measures whether you have a type of antibody that could block gene therapy from working as intended, which could also impact safety.
Antibodies are part of the immune system. Their job is to help protect against illness, including viruses, by blocking their effect on the body. When someone has been exposed to a virus, the body’s immune system creates specific antibodies that remember how to fight it in the future.
Vectors—the delivery tools in gene therapy—are similar to viruses that occur naturally. Much like viruses, they can successfully deliver materials to specific cells in the body but have been changed in a laboratory to prevent them from multiplying or causing an illness.
If someone has been previously exposed to a virus similar to a gene therapy’s vector, the immune system’s antibodies may prevent the gene therapy from doing its job and could cause harmful side effects. Using a blood test to look for high levels of the specific antibodies that recognize the vector is important; if levels are too high, treatment may not be possible. Scientists are in the early stages of research to address this, and are working hard to see if there's a way around the specific antibodies that recognize the vector.
Remember, genetic and preexisting antibody testing are only 2 elements that may be required to determine eligibility for gene therapy—your doctor can provide more information about additional requirements for specific treatments.
Currently designed as a one-time treatment
Currently, gene therapies can only be taken once. After treatment, the antibodies created in response to the vector may prevent the treatment from working if given a second time.
Common gene therapy assessments in clinical trials
The goal of gene therapy research in Duchenne is to see whether it can help slow or stabilize the disease. Researchers are looking at whether or not gene therapy can help the body make a different but working version of dystrophin. Clinical trials explore the safety of a potential gene therapy and assess whether it is working as intended. Common areas researchers assess include:
Safety
Researchers follow clinical trial participants carefully—often for years—to assess the potential side effects.
Protein Expression
The goal of gene therapy is to instruct the target cells to make a new protein. Researchers measure this using different techniques to assess protein expression, which demonstrates if the protein is being made and if it’s in the right place in the cells.
Scientists collect and look inside the cells affected by the genetic disease to measure protein expression. First, they look to see if the new protein was created. Western blot is a common test used to measure how much of a specific protein is in a collection of cells. Second, they often use an immunofluorescence test to confirm whether the new protein is in the right location inside the cells.
Taken together, tests like Western blot and immunofluorescence help researchers determine whether the gene therapy is working inside the cells as intended.
Muscle Function
Clinical trials can also test how a person’s muscles perform before and after treatment.
Some of the tests used to assess this may include:
- The North Star Ambulatory Assessment, also called North Star or NSAA—a test that evaluates a person's ability to perform 17 everyday activities, such as standing, walking, rising from the floor, hopping, jumping, climbing, and running
- The Performance of Upper Limb module, often abbreviated as PUL—a test used to see how well a person can use their shoulders, arms, wrists, and hands
- The 6-minute walk test, often written as 6MWT—a test used to determine how far a person can walk in 6 minutes on a hard, flat surface
Researchers use these tests to see if the person's muscles functioned better, stayed the same, or worsened after treatment. To determine this, they may look at:
- How a participant's muscles performed before (called baseline) and after treatment
- How a person's muscle performance compared to those of someone who wasn't treated (sometimes called a placebo group)
- How a participant's muscle performance compared to individuals who were not in the trial (sometimes called an external control group)
 Test your knowledge of gene therapy.
Test your knowledge of gene therapy.


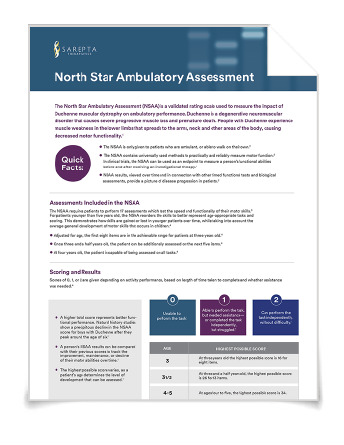 Read more about the NSAA.
Read more about the NSAA.